GEORGIAN RADIOLOGY CONSULTANTS
Medical Imaging is convenient, fast and easy.

Review: Bone Mineral Densitometry
Normal Bone

Osteoporosis

Severe Osteoporosis

Bone Mineral Densitometry (BMD)
What is Bone Mineral Densitometry?
Osteoporosis is a disease characterized by low bone mass and deterioration of bone tissue. This leads to increased bone fragility and risk of fracture, particularly of the hip, spine and wrist. Osteoporosis is often known as “the silent thief” because bone loss occurs without symptoms. Bone densitometry measures the bone mineral content in various sites of the body, allowing a physician to diagnose osteoporosis and assess a patient’s risk of suffering bone fractures.
Risk Factors
Osteoporosis Canada recommends all postmenopausal women and men over 50 be assessed for risk factors for osteoporosis.
Major Risk Factors:
- Age 65 or older
- Vertebral compression fracture
- Fracture with minimal trauma after age 40
- Family history of osteoporotic fracture (especially if your mother had a hip fracture)
- Long-term (more than 3 months continuously) use of glucocorticoid therapy such as prednisone
- Medical conditions (such as celiac disease, Crohn’s disease) that inhibit absorption of nutrients
- Primary hyperparathyroidism
- Tendency to fall
- Osteopenia apparent on X-ray
- Hypogonadism (low testosterone in men, loss of menstrual periods in younger women)
- Early menopause (before age 45)
Minor Risk Factors:
- Rheumatoid arthritis
- Hyperthyroidism
- Prolonged use of anticonvulsants
- Prolonged heparin use
- Body weight less than 57 kg (125 lbs.)
- If your present weight is more than 10% below your weight at age 25
- Low calcium intake
- Excess caffeine (consistently more than 4 cups a day of coffee, cola or some energy drinks)
- Excess alcohol (consistently more than 2 drinks a day)
- Smoker
- Chronic diseases (Liver, COPD, MM, Cancer)
Men & Osteoporosis
Osteoporosis is often considered to be a woman’s disease. Osteoporosis is less common in men than in women for a number of reasons. Men have greater peak bone mass and do not experience the accelerated bone loss women do at menopause. As well, they generally do not live as long and are less likely to fall than elderly women.
Although more common in women, osteoporosis is a serious health issue for men. As with the decline of estrogen levels in women, lower testosterone levels in men can lead to an increase in bone loss. The decline is more gradual in men and is not universal. At least one in eight men over 50 has the disease.
According to a Canadian study of healthy men and women, the number of fractures of the spine is similar in men and women over the age of 50. Elderly men account for almost 30% of hip fracture cases, but men are more likely to die after a hip fracture. Fractures, or broken bones, in both men and women, often lead to significant physical and emotional problems. If you have had a fracture, the chances of having another one increase greatly.
Screening Recommendations
It is recommended that all patients, male or female, over the age of 65 have a screening bone densitometry examination. Patients under the age of 65 should have a baseline screening study if they have one major, or two minor risk factors.
Follow-up studies are dependent on the results of the screening examination. Patients with normal bone densities are considered low risk and can only be re-tested every three years. Patients with reduced bone densities, or risk factors for osteoporosis, are considered high risk and can be retested more frequently. Recommendations for follow-up are included in our reports.
Results
In BMD test results, the patient’s bone density is compared to the bone density of an average young adult. An actual bone density measurement in grams per cm2 is obtained. A T-score is then calculated that compares the density of the patient’s bones (spine, femoral neck, trochanter, and total femur) relative to this average. While some bone loss with aging is considered normal, making such comparisons helps determine whether the patient is losing bone more rapidly than expected.
The T-score is expressed in units referred to as standard deviations (SDs). These SD units tell us how far the patient differs (or deviates) from what is considered normal for a young adult. Below normal is always indicated with a minus (-) sign. According to World Health Organization (WHO) classifications, for postmenopausal patients over 50, a T-score below 2.5 SDs indicates osteoporosis and a score between 1 and 2.5 SDs indicates osteopenia. Normal bone density is no more than 1 SD below the young adult normal value. For female patients under 50, and all male patients, a T-score below 2.5 SDs indicates reduced bone density, with normal bone density being anything above this.
BMD test results and the WHO classifications are only part of the picture in determining the risk for fracture. In addition to the BMD results, the Radiologist will consider factors such as age, gender, fracture history, family history and glucocorticoid (steroid) use to determine the 10-year absolute fracture risk.
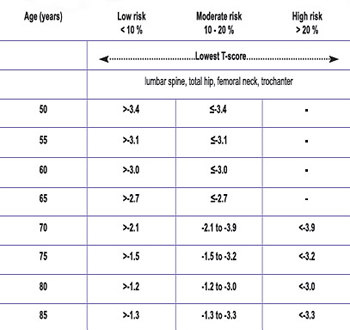
Tables 1 and 2 are used to determine whether the 10-year fracture risk is low, moderate or high, considering the BMD results, age and gender. Other clinical factors, particularly a fragility fracture after age 40 or glucocorticoid use for more than three months, substantially elevate the fracture risk. The presence of either of these factors will increase the 10-year risk of fracture to the next level. If both of these particular factors were present, the patient would be considered at high risk regardless of the BMD result.
Table 1: 10-year fracture risk for women
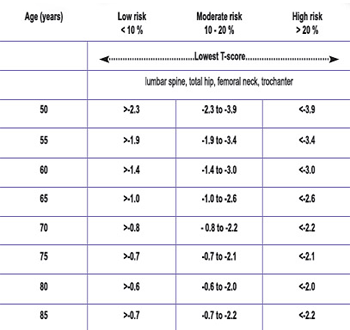
Table 1: 10-year fracture risk for men
Useful Links
MOHLTC Website: http://www.health.gov.on.ca/english/public/pub/ohip/bone_density.html
Osteoporosis Canada Website: http://www.osteoporosis.ca/
Bone Mineral Density Requisition Form
Bone Health Assessment
Bone health assessments are targeted towards patients under investigation for vertebral compression fracture. We offer convenient and comprehensive appointments including nuclear medicine bone scan, x-rays, and/or densitometry to offer a holistic picture of your patient’s bone health, in one appointment. The assessment may be followed by a later consultation for vertebroplasty with our Interventional Radiologists if desired.
Use our Bone Health Assessment Requisition Form to streamline the process from diagnosis to treatment.
Nuclear Medicine
We are offering nuclear cardiac services such as Myocardial Perfusion Imaging (MPI) with pharmacological (Persantine) stressing and MUGAs .
We are also offering an array of non-cardiac nuclear diagnostic imaging namely Bone Flow and Scan (specific site), Total Body Bone scan, SPECT, Hepatobiliary Flow and Scan, RBC Liver Scan, Liver/Spleen Flow and Scan, Renal Flow and Scan, Salivary Scan, Parathyroid Scan, Perfusion Brain Scan.
Review: Integrated Prenatal Screening (IPS)
Integrated Prenatal Screening (IPS)
Screening Recommendations
The Society of Gynecology and Obstetrics of Canada recommends that “all pregnant women in Canada, regardless of age, should be offered, through an informed consent process, a prenatal screening test for the most common clinically significant fetal aneuploidies in addition to a second trimester ultrasound for dating, growth, and anomalies.”
The most common method of fulfilling this is to do an Integrated Prenatal Screening (IPS) testing combined with an 18-20-week ultrasound.

Integrated Prenatal screening is a three-step process.
- Nuchal translucency (NT) and early anatomy ultrasound. This is done at 11-13 weeks, but ideally should be scheduled between 11 weeks 5 days and 13 weeks 6 days. The gestational age is confirmed. The tissue at the back of the fetus’s neck (NT) is measured. (Babies with trisomy 21 and other aneuploidies tend to accumulate more fluid here)
- The first blood test must be done on the same day. Your patient must have the correct paperwork with them to complete the test. This test measures proteins in the blood and is used to modify the risk rating.
- The second blood test is done between 15 – 18 weeks.
Results
Results are labeled as either screen positive or negative.
- Screen Positive – If the results indicate a greater than 1/200 risk of Down Syndrome or a 1/100 risk of Trisomy 18 or 13 they are considered positive. 2% of all tests will be positive. Most will be false positive. Close to 90% of the pregnancies affected with Down Syndrome will screen positive (true positive).
- Screen Negative – A screen negative result indicates the chance of Down Syndrome is less than 1/200. More than 99% of pregnancies with normal 21, 18 and 13 chromosomes will screen negative. Please remember that 10% of pregnancies with Down Syndrome will also screen negative (false negative).
Other Benefits
- Placental Function – The same biochemical factors that are used in IPS testing have been found to reflect placental function and can identity a group of patients at risk for placental insufficiency. These patients have higher rates of IUGR, SGA, premature delivery and fetal demise. This group of patients can be further stratified by examining the maternal uterine arteries.
The IPS is considered to be false positive when both aneuploidy (trisomy 21, 18 and 13) and neural tube defects are excluded. Adverse pregnancy outcomes have been associated with false positive IPS with the following abnormal maternal serum markers:
1st trimester 10-13 weeks blood work:
low papp-a (<0.35 MOM)
hCG >5.0 MOM
inhibin A >3.0 MOM
2nd trimester 15-20 weeks blood work:
AFP >2.0 MOM
In the setting of a false positive IPS described above, measurement of maternal uterine artery Doppler has been shown to identify a group of pregnant women with the highest risk of adverse pregnancy outcomes. Uterine artery Doppler is typically performed between 18-22 weeks and an abnormal Doppler measurement with the maternal uterine artery Pulsatility Index (PI) > 1.45 suggests there is high risk for subsequent placental insufficiency. This patient will require early referral to an obstetrician. A normal PI is reassuring but should be followed with a third trimester ultrasound for fetal growth.
We ask that if you receive an abnormal IPS result, proceed with the 18 to 20-week ultrasound already booked, refer to genetic counselling for further testing, and refer the patient for uterine artery Doppler (18-22 weeks). In Barrie, this test is currently offered at the RVH but services will expand to the local clinics if demand is high. Please fax the IPS results with the ultrasound requisition.
Uterine Artery Doppler should also be considered in women at risk of placental pathology with current obstetric risk factors (pre-existing hypertension, gestational hypertension, thrombophilia, pre-existing renal disease and Type 1 Diabetes with vascular complications) as well as past obstetric risk factors (early onset gestational hypertension, placental abruption, IUGR and stillbirth).
Uterine Doppler will not be done in low risk pregnancies as it is not proven as a useful tool.
- Twin Pregnancy – If your patient is having twins, the chronicity can be most accurately assessed at an early ultrasound. This will affect your patient’s management throughout the pregnancy. Identical twins are at higher risk of complications. Monochorionic/monoamniotic and monochorionic/diamniotic pregnancies need early referral to obstetrics. Blood tests are not accurate in twins or triplets so the best screening test is the nuchal translucency which is unique to each baby.
Useful Links
The Society of Obstetrics and Gynecology of Canada 2007 Guidelines on Screening for aneuploidy: http://www.sogc.org/media/pdf/advisories/JOGC-feb_07-CPG.pdf
Mt Sinai IPS website: http://www.mountsinai.on.ca/care/pdmg/tests/ips
Screening Guide for Patients: Click here to download
Reference Guide for Health Care Providers: Click here to download
Review: Thyroid Nodules
Thyroid Nodules
Epidemiology
Thyroid nodules are extremely common in the population. Approximately 50% of the adult population have thyroid nodules on ultrasound. Fortunately, only 3-7% of these nodules are malignant.
Nodules are more common in:
- Elderly persons
- Women
- Iodine deficiency
- History of radiation exposure

Risk factors for carcinoma include:
- Age less than 20 years or more than 60 years
- History of neck irradiation
- Family history of thyroid cancer
- Male sex
- Previous diagnosis of type 2 MEN
Incidence of Thyroid cancer has increased over the last 30 years. The cause for this is uncertain but may be related to:
- Better diagnosis
- More FNA with US guidance (increased accuracy)
- Rise in radiation exposure in the general public
Ultrasound
Management
The decision to biopsy is based on the patient’s risk factors, the size and appearance of the nodule and the presence of suspicious cervical lymph nodes. In general, only solid nodules larger than 10mm should be considered for biopsy. Other nodules should be followed by ultrasound in 6-12 months and regularly thereafter. If a nodule is thought to be enlarging, then follow-up can be performed sooner.
Useful Links
The 2009 American Thyroid Association Guidelines for Management of Thyroid Nodules and Differentiated Thyroid Cancer: Progress on the Road from Consensus- to Evidence-Based Practice are available through this link: http://www.liebertonline.com/doi/pdf/10.1089/thy.2009.1601
American Association of Clinical Endocrinologists Medical Guidelines for Clinical Practice for the diagnosis and management of Thyroid Nodules. 2006. https://www.aace.com/files/thyroid-guidelines.pdf
Requisition Form
Before coming to one of our clinics, please remember:
To view the form, you will need Adobe Reader. You may download Adobe Reader for free at www.adobe.com. Please bring your completed form with you to our office at the time of your visit.
Book Your Ultrasound, BMD, Nuclear Medicine Appointment
To book an appt, please FAX the requisition to 705-726-8056
Or for your Ultrasound, BMD, Nuclear Medicine Appointment BOOK HERE with your name, phone number, and a clear copy of your requisition.
X rays are walk in only. Please do not email/fax X ray requisitions.
Things To Remember
Before coming to one of our clinics, please remember:
1. Your valid health card.
2. A signed requisition order or high-risk requisition order from your doctor.
3. Wearing masks is optional but encouraged.
View Our Articles
Find out more about our services by reading reading our blogs below.

Visit Georgian Radiology’s new location in Little Lake
Georgian Radiology is pleased to announce the opening of our newest clinic in the Little Lake Health Centre on June 22, 2015. This new location will allow us to expand our services in order to

Georgian Radiology
In Ontario, very few, if any medical practices are truly full-service – in other words, able to provide anything and everything that any one patient might require, from ultrasound to stress testing to a bone
